Kelly Ripa Diagnoses Husband Mark Consuelos with Narcolepsy

In one of our most popular stories, Live! with Kelly and Michael co-host Kelly Ripa diagnosed herself with misophonia (literally “hatred of sound”).
Now she’s telling Jimmy Kimmel that she believes her husband, Alpha House actor Mark Consuelos, has narcolepsy, or what she refers to as “Marcolepsy.”
Consuelos can apparently fall asleep at the drop of a hat, even at unusual places, such as award shows and even in the bathroom of Live! executive producer Michael Gelman’s home during a dinner party!
Kimmel understands what Ripa is talking about, as he himself was diagnosed as having narcolepsy in 2003. He is currently treated with a stimulant medication called Provigil (Generic name: Modafinil)
What is Narcolepsy?
Source: National Institute of Neurological Disorders and Stroke
Narcolepsy is a chronic brain disorder that involves poor control of sleep-wake cycles. People with narcolepsy experience periods of extreme daytime sleepiness and sudden, irresistible bouts of sleep that can strike at any time. These “sleep attacks” usually last a few seconds to several minutes.
Narcolepsy can greatly affect daily activities. People may unwillingly fall asleep while at work or at school, when having a conversation, playing a game, eating a meal, or, most dangerously, when driving or operating other types of machinery. In addition to daytime sleepiness, other major symptoms may include cataplexy (a sudden loss of voluntary muscle tone while awake that makes a person go limp or unable to move), vivid dream-like images or hallucinations, as well as total paralysis just before falling asleep or just after waking-up.
 Contrary to common beliefs, people with narcolepsy do not spend a substantially greater proportion of their time asleep during a 24-hour period than do normal sleepers. In addition to daytime drowsiness and uncontrollable sleep episodes, most individuals also experience poor sleep quality that can involve frequent waking during nighttime sleep, and other sleep disorders.
Contrary to common beliefs, people with narcolepsy do not spend a substantially greater proportion of their time asleep during a 24-hour period than do normal sleepers. In addition to daytime drowsiness and uncontrollable sleep episodes, most individuals also experience poor sleep quality that can involve frequent waking during nighttime sleep, and other sleep disorders.
Narcolepsy affects both males and female equally and appears throughout the world. Symptoms often start in childhood or adolescence, but can occur later in life. The condition is life-long. Narcolepsy is not rare, but it is an under-recognized and underdiagnosed condition. Narcolepsy with cataplexy is estimated to affect about one in every 3,000 Americans.
What are the symptoms?
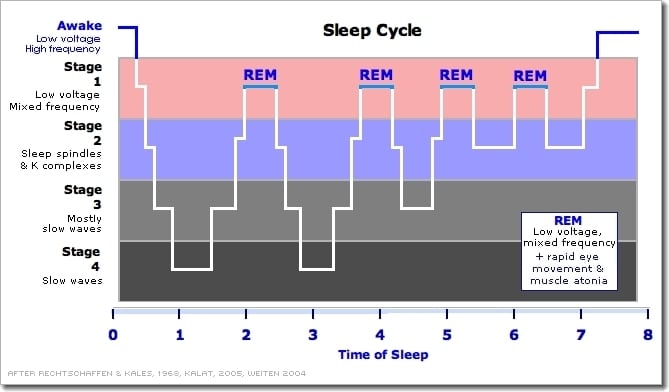
People with narcolepsy experience various types of day- and nighttime sleep problems that are associated with REM sleep disturbances that tend to begin subtly and may change dramatically over time. The most common major symptom, other than excessive daytime sleepiness (EDS), is cataplexy, which occurs in about 70 percent of all people with narcolepsy. Sleep paralysis and hallucinations are somewhat less common. Only 10 to 25 percent of affected individuals, however, display all four of these major symptoms during the course of their illness.
Excessive daytime sleepiness (EDS)
EDS, the symptom most consistently experienced by almost all individuals with narcolepsy, is usually the first to become clinically apparent. Generally, EDS interferes with normal activities on a daily basis, whether or not individuals had sufficient sleep at night. People with EDS describe it as a persistent sense of mental cloudiness, a lack of energy, a depressed mood, or extreme exhaustion. Some people experience memory lapses, and many have great difficulty maintaining their concentration while at school, work, or home. People tend to awaken from such unavoidable sleeps feeling refreshed and finding that their drowsiness and fatigue subsides for an hour or two.
It should be noted that EDS can be the result of a wide range of medical conditions, including other sleep disorders such as sleep apnea, various viral or bacterial infections, mood disorders such as depression, and chronic illnesses such as anemia, congestive heart failure, and rheumatoid arthritis that disrupt normal sleep patterns.
Cataplexy
Cataplexy is a sudden loss of muscle tone while the person is awake that leads to feelings of weakness and a loss of voluntary muscle control. Attacks can occur at any time during the waking period. Cataplectic attacks vary in duration and severity. The loss of muscle tone can be barely perceptible, involving no more than a momentary sense of slight weakness in a limited number of muscles, such as mild drooping of the eyelids. The most severe attacks result in a complete loss of tone in all voluntary muscles, leading to physical collapse during which individuals are unable to move, speak, or keep their eyes open. But even during the most severe episodes, people remain fully conscious, a characteristic that distinguishes cataplexy from seizure disorders.
Sleep paralysis
The temporary inability to move or speak while falling asleep or waking is similar to REM-induced inhibitions of voluntary muscle activity. This natural inhibition usually goes unnoticed by people who experience normal sleep because it occurs only when they are fully asleep and entering the REM stage at the appropriate time in the sleep cycle. The attacks usually last a few seconds or minutes.
Hallucinations
Hallucinations can accompany sleep paralysis and occur when people are falling asleep, waking, or during sleep. Referred to as hypnagogic hallucinations when occurring during sleep onset and as hypnopompic hallucinations when occurring during waking, these images are unusually vivid, seem real, and can be frightening.
What causes narcolepsy?
Narcolepsy may have several causes. Most people with narcolepsy have low levels of the neurotransmitter hypocretin, which promotes wakefulness. Neurotransmitters are chemicals that neurons produce to communicate with each other and to regulate biological processes.
How is narcolepsy diagnosed?
A physical examination and complete medical history are essential for diagnosis and treatment. A sleep journal, noting the times of sleep and symptoms over a one-to-two-week period, can also be useful.
Two tests in particular are essential in confirming a diagnosis of narcolepsy: the polysomnogram (PSG) and the multiple sleep latency test (MSLT):
- The PSG is an overnight test that records heart and respiratory rates, electrical activity in the brain using electroencephalography, and nerve activity in muscles through electromyography while the individual is asleep . A PSG can help reveal whether REM sleep occurs at abnormal times in the sleep cycle and can rule out the possibility that an individual’s symptoms result from another condition, such as sleep apnea.
- The MSLT is performed during the day to measure a person’s tendency to fall asleep and to determine whether isolated elements of REM sleep intrude at inappropriate times during the waking hours.
The sleep latency test measures the amount of time it takes for a person to fall asleep. As part of the test, an individual is asked to take four or five short naps usually scheduled 2 hours apart over the course of a day. Because sleep latency periods are normally 12 minutes or longer, a latency period of 8 minutes or less suggests a disorder of excessive daytime sleepiness. The MSLT also measures heart and respiratory rates, records nerve activity in muscles, and pinpoints the occurrence of abnormally timed REM episodes through EEG recordings. If a person enters REM sleep either at the beginning or within a few minutes of sleep onset during at least two of the scheduled naps, this is considered an indication of narcolepsy.
What treatments are available?
Narcolepsy cannot yet be cured, but some of the symptoms can be treated with medicines and lifestyle changes. When cataplexy is present, the loss of hypocretin is believed to be irreversible and life-long. But EDS and cataplexy can be controlled in most individuals with drug treatment. Modafinil and sodium oxybate are two drugs that have been approved by the U.S. Food and Drug Administration for the treatment of narcolepsy.
What behavioral strategies help people cope with symptoms?
Many individuals take short, regularly scheduled naps at times when they tend to feel sleepiest.
Improving the quality of nighttime sleep can combat EDS and help relieve persistent feelings of fatigue. Among the most important common-sense measures people can take to enhance sleep quality are:
- maintain a regular sleep schedule—go to bed and wake up at the same time every day
- avoid alcohol and caffeine-containing beverages for several hours before bedtime
- avoid large, heavy meals just before bedtime
- avoid smoking, especially at night
- maintain a comfortable, adequately warmed bedroom environment, and
- engage in relaxing activities such as a warm bath before bedtime.
Exercising for at least 20 minutes per day at least 4 or 5 hours before bedtime also improves sleep quality and can help people with narcolepsy avoid gaining excess weight.























0 comments