Ann B. Davis’s Death: A Cautionary Tale for Seniors

She was the center square of The Brady Bunch tic-tac-toe grid. As the good-natured housekeeper Alice Nelson, Ann B. Davis was an important part of the “cement” that turned two previously separate families into one. The two-time Emmy-winning actress died this week at the age of 88.
Davis died after sustaining a head injury after a fall. The injury caused a subdural hematoma (see below) and she did not regain consciousness.
With the news of her death, former co-stars quickly took to social media to express their love for her:
“I was reflecting throughout the day yesterday about one of the first times I met her. She was already a big star when she joined ‘The Brady Bunch,’ won a couple of Emmys with ‘The Bob Cummings Show,’ and I knew that this was someone I wanted to pay attention to but she had a wicked sense of humor.”
— Barry Williams“I’m so shocked & saddened to learn my dear friend & colleague Ann B Davis died today.I spoke with her a few months ago & she was doing great”
— Florence Henderson
What is a Subdural Hematoma?
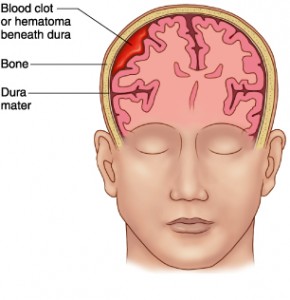 A subdural hematoma is caused by bleeding that takes place due to the rupture of one or more of the blood vessels (typically veins) that travel through the subdural space, located between the dura mater, which adheres to the skull, and the arachnoid mater enveloping the brain. Acute bleeds develop after high speed acceleration or deceleration injuries. Acute subdural hematomas are among the deadliest of all head injuries. The bleeding fills the brain area very rapidly, compressing brain tissue.
A subdural hematoma is caused by bleeding that takes place due to the rupture of one or more of the blood vessels (typically veins) that travel through the subdural space, located between the dura mater, which adheres to the skull, and the arachnoid mater enveloping the brain. Acute bleeds develop after high speed acceleration or deceleration injuries. Acute subdural hematomas are among the deadliest of all head injuries. The bleeding fills the brain area very rapidly, compressing brain tissue.
Symptoms are similar to those of anyone having a stroke:
- Confused speech
- Difficulty with balance or walking
- Headache
- Lethargy or confusion
- Loss of consciousness
- Nausea and vomiting
- Numbness
- Seizures
- Slurred speech
- Visusal disturbances
- Weakness
How big an issue are falls in the elderly?
Falls in the elderly is a major health issue, especially as the baby-boomer generation ages.
How big is the problem?
According to the CDC:
- One out of three older adults (those aged 65 or older) falls each year but less than half talk to their healthcare providers about it.
- Among older adults, falls are the leading cause of both fatal and nonfatal injuries.
- In 2010, 2.3 million nonfatal fall injuries among older adults were treated in emergency departments and more than 662,000 of these patients were hospitalized.
- In 2010, the direct medical costs of falls, adjusted for inflation, was $30 billion.
What outcomes are linked to falls?
- Twenty to thirty percent of people who fall suffer moderate to severe injuries such as lacerations, hip fractures, or head traumas. These injuries can make it hard to get around or live independently, and increase the risk of early death.
- Falls are the most common cause of traumatic brain injuries (TBI).
- In 2000, 46% of fatal falls among older adults were due to TBI.
- Most fractures among older adults are caused by falls. The most common are fractures of the spine, hip, forearm, leg, ankle, pelvis, upper arm, and hand.
- Many people who fall, even if they are not injured, develop a fear of falling. This fear may cause them to limit their activities, which leads to reduced mobility and loss of physical fitness, and in turn increases their actual risk of falling.
Who is at risk?
- Men are more likely to die from a fall. After adjusting for age, the fall fatality rate in 2004 was 49% higher for men than for women.
- Women are 67% more likely than men to have a nonfatal fall injury, with fall-related fractures twice as high for women as for men. Women account for over 70% of hospital admissions for hip fractures.
- The risk of being seriously injured in a fall increases with age. Adults over 85 were four to five times more likely to fall than adults 65 to 74.
- Nearly 85% of deaths from falls in 2004 were among people 75 and older.
- People 75 and older who fall are four to five times more likely to be admitted to a long-term care facility for a year or longer.
- There is little difference in fatal fall rates between whites and blacks, ages 65 to 74 . After age 75, white men have the highest fatality rates, followed by white women, black men, and black women.
How can older adults prevent falls?
Older adults can take several steps to protect their independence and reduce their risk of falling. They can:
- Exercise regularly; exercise programs like Tai Chi that increase strength and improve balance are especially good.
- Ask their doctor or pharmacist to review their medicines–both prescription and over-the counter–to reduce side effects and interactions.
- Have their eyes checked by an eye doctor at least once a year.
- Improve the lighting in their home, and outdoors on walkways around the home.
- Reduce hazards inside and outside their home that can lead to falls.





















0 comments