Death of a Ghostbuster: Harold Ramis Gone

Harold Ramis, probably best known for his role as Dr. Egon Spengler from Ghostbusters, has died at the age of 69. Ramis, who also appeared in Stripes and was the writer/director for Cadddyshack, Groundhog Day and Analyze This died of a rare autoimmune disease called autoimmune inflammatory vasculitis.
His wife, Erica Mann Ramis told the Chicago Tribune that Ramis was diagnosed in May 2010, when he was diagnosed with an infection. This lead to complications related to his autoimmune disease. The illness left him unable to walk, but he was able to relearn the skill. He suffered a relapse of the disease in 2011.
Many of his friends immediately took to social media to express their feelings about their lost friend:
“Deeply saddened to hear of the passing of my brilliant, gifted, funny friend, co-writer/performer and teacher Harold Ramis.”
— Ghostbusters co-star Dan Aykroyd
“Harold Ramis and I together did ‘The National Lampoon Show’ off-Broadway, ‘Meatballs,’ ‘Stripes,’ ‘Caddyshack,’ ‘Ghostbusters’ and ‘Groundhog Day.’ He earned his keep on this planet. God bless him.”
— Bill Murray
What is autoimmune inflammatory vasculitis?
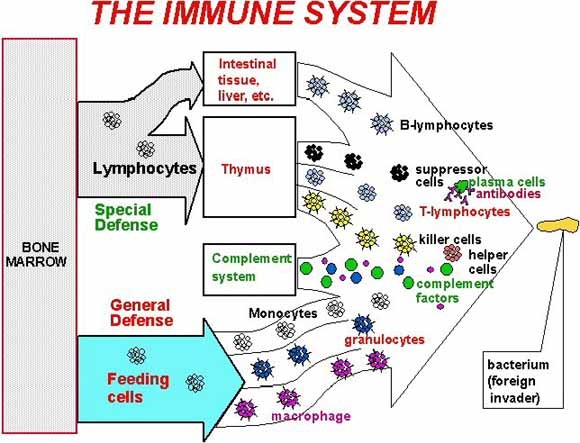
Autoimmune inflammatory vasculitis is one of more than 80 diseases which occur as a result of the immune system attacking the body’s own organs, tissues, and cells.
Normally the immune system’s white blood cells help protect the body from harmful substances, called antigens. Examples of antigens include bacteria, viruses, toxins, cancer cells, and blood or tissues from another person or species. The immune system produces antibodies that destroy these harmful substances.
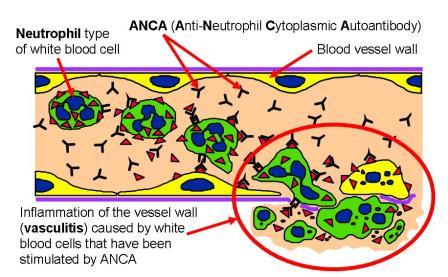 In patients with an autoimmune disorder, the immune system can’t tell the difference between healthy body tissue and antigens. The result is an immune response by infection-fighting white blood cells that destroys normal body tissues.
In patients with an autoimmune disorder, the immune system can’t tell the difference between healthy body tissue and antigens. The result is an immune response by infection-fighting white blood cells that destroys normal body tissues.
Autoimmune vasculitis can be seen alone or as part of a number of different autoimmune diseases (see chart below). The target for the mistaken inflammation is blood vessels throughout the body, and can have different effects depending on the size and the location of the affected blood vessels.
| Types of Vasculitis | |
|---|---|
| Largest arteries: aorta and major branches | Giant cell arteritis Takayasu’s arteritis Aortitis in Cogan’s syndrome Aortitis in spondylarthropathies Isolated aortitis |
| Medium-sized arteries | Kawasaki disease Polyarteritis nodosa |
| Small and medium-sized arteries | ANCA-associated vasculitis Granulomatosis with polyangiitis (former name: Wegener’s granulomatosis) Microscopic polyangiitis Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) Primary angiitis of the central nervous system |
| Small arteries | IgA Vasculitis (Henoch-Schönlein) Vasculitis related to rheumatoid arthritis, systemic lupus erythematosus and Sjögren’s syndrome Cryoglobulinemic vasculitis Anti-GBM disease (Goodpasture’s) Drug-induced vasculitis |
| Arteries and veins of various sizes | Behcet’s disease Relapsing polychondritis |
| Abbreviations: ANCA, antineutrophil cytoplasmic antibodies; GBM, glomerlular basement membrane. | |
Source: American College of Rheumatology
What are the symptoms of autoimmune vasculitis?
Symptoms of vasculitis include non-specific symptoms such a fever, body aches, joint and muscle pain, reduced appetite, and weight loss.
More specific symptoms depend on the size and location of the affected blood vessels and can include:
Affected Body Part |
Symptoms |
| Kidney | Brown, tea-colored urine from blood leaking into the urine |
| Joints | Joint pain or swelling |
| Lungs | Heavy cough, often mistaken for pneumonia, coughing up blood |
| Skin | Red or purple spots , itching, hives, rash |
| Sinus/Nose | Runny nose that get worse and worse, nose pain, trouble breathing through nose |
| Trachea | Shortness of breath |
| Gastrointestinal Tract | Stomach pain, or blood in stool |
| Eyes | Red, painful eyes, blurry vision, headaches |
| Ears | Hearing Problems or Hearing Loss |
Source: UNC Health Care
How is autoimmune vasculitis treated?
The goal of treatment is to reduce symptoms, and control the autoimmune process while maintaining the body’s ability to fight disease.
Which treatments are used depends on the specific disease and the specific symptoms.
Medicines are often prescribed to control or reduce the immune system’s response. They are called immunosuppressive medicines. Such medicines may include corticosteroids (such as prednisone) and nonsteroid drugs such as azathioprine, cyclophosphamide, rituximab, or Methotrexate.
The outcome depends on the disease. Most autoimmune diseases are chronic, but many can be controlled with treatment.
For more information, click here to go to the Resounding Health Casebook on the topic.























0 comments