Meet an American Idol contestant with Tourette’s and Asperger’s Syndromes

Last night’s American Idol episode introduced us to James Durbin, a 21-year-old singer from Santa Cruz, CA. Durbin has known quite a bit of adversity in his short life; his musician father died of a drug overdose when James was 9 years old and he has been diagnosed with both Tourette and Asperger’s Syndromes. With a voice somewhat reminiscent of Idol Season 8 runner-up Adam Lambert, Durbin wowed the judges with his soaring range and emotional performance of “Shook Me All Night Long” and Aerosmith’s “Dream On.” After his performance, Durbin admitted to the judges that when he sings, his Tourette’s “all goes away.”
Asperger’s Syndrome (AS) is a developmental disorder which is part of the Autistic Spectrum Disorders (ASD) - a group of neurological conditions characterized by a greater or lesser degree of impairment in communication and social skills, as well as repetitive or restrictive patterns of thought and behavior. Individuals with AS are differentiated from others with autism in that they retain their early language and cognitive skills, and tend to be less severely impaired than those with autism. We have covered Asperger’s syndrome in previous stories about Temple Grandin and Amazing Race contestant Zev Glassenberg . Readers can go to those stories to find out more information about that disease.
What is Tourette Syndrome? (Source: NINDS)
Tourette syndrome (TS) is a neurological disorder characterized by repetitive, stereotyped, involuntary movements and vocalizations called tics. The disorder is named for Dr. Georges Gilles de la Tourette, the pioneering French neurologist who in 1885 first described the condition in an 86-year-old French noblewoman.
The early symptoms of TS are almost always noticed first in childhood, with the average onset between the ages of 7 and 10 years. TS occurs in people from all ethnic groups; males are affected about three to four times more often than females. It is estimated that 200,000 Americans have the most severe form of TS, and as many as one in 100 exhibit milder and less complex symptoms such as chronic motor or vocal tics or transient tics of childhood. Although TS can be a chronic condition with symptoms lasting a lifetime, most people with the condition experience their worst symptoms in their early teens, with improvement occurring in the late teens and continuing into adulthood.
What are the symptoms?
Tics are classified as either simple or complex. Simple motor tics are sudden, brief, repetitive movements that involve a limited number of muscle groups. Some of the more common simple tics include eye blinking and other vision irregularities, facial grimacing, shoulder shrugging, and head or shoulder jerking. Simple vocalizations might include repetitive throat-clearing, sniffing, or grunting sounds. Complex tics are distinct, coordinated patterns of movements involving several muscle groups. Complex motor tics might include facial grimacing combined with a head twist and a shoulder shrug. Other complex motor tics may actually appear purposeful, including sniffing or touching objects, hopping, jumping, bending, or twisting. Simple vocal tics may include throat-clearing, sniffing/snorting, grunting, or barking. More complex vocal tics include words or phrases. Perhaps the most dramatic and disabling tics include motor movements that result in self-harm such as punching oneself in the face or vocal tics including coprolalia (uttering swear words) or echolalia (repeating the words or phrases of others). Some tics are preceded by an urge or sensation in the affected muscle group, commonly called a premonitory urge. Some with TS will describe a need to complete a tic in a certain way or a certain number of times in order to relieve the urge or decrease the sensation.
Tics are often worse with excitement or anxiety and better during calm, focused activities. Certain physical experiences can trigger or worsen tics, for example tight collars may trigger neck tics, or hearing another person sniff or throat-clear may trigger similar sounds. Tics do not go away during sleep but are often significantly diminished.
What is the course of TS?
Tics come and go over time, varying in type, frequency, location, and severity. The first symptoms usually occur in the head and neck area and may progress to include muscles of the trunk and extremities. Motor tics generally precede the development of vocal tics and simple tics often precede complex tics. Most patients experience peak tic severity before the mid-teen years with improvement for the majority of patients in the late teen years and early adulthood. Approximately 10 percent of those affected have a progressive or disabling course that lasts into adulthood.
What causes TS?
Although the cause of TS is unknown, current research points to abnormalities in certain brain regions (including the basal ganglia, frontal lobes, and cortex), the circuits that interconnect these regions, and the neurotransmitters (dopamine, serotonin, and norepinephrine) responsible for communication among nerve cells. Given the often complex presentation of TS, the cause of the disorder is likely to be equally complex.
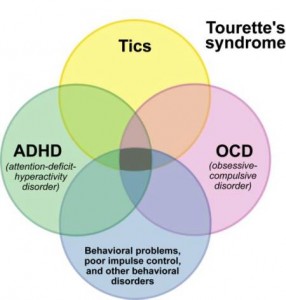 What disorders are associated with TS?
What disorders are associated with TS?
Many with TS experience additional neurobehavioral problems including inattention; hyperactivity and impulsivity (attention deficit hyperactivity disorder—ADHD) and related problems with reading, writing, and arithmetic; and obsessive-compulsive symptoms such as intrusive thoughts/worries and repetitive behaviors.
How is TS treated?
Because tic symptoms do not often cause impairment, the majority of people with TS require no medication for tic suppression. However, effective medications are available for those whose symptoms interfere with functioning. Neuroleptics are the most consistently useful medications for tic suppression; a number are available but some are more effective than others (for example, haloperidol and pimozide). Unfortunately, there is no one medication that is helpful to all people with TS, nor does any medication completely eliminate symptoms.
For more information about Tourette Syndrome, click here to go to the Resounding Health Casebook on the topic.























4 Comments